This job is closed
We regret to inform you that the job you were interested in has been closed. Although this specific position is no longer available, we encourage you to continue exploring other opportunities on our job board.
About the position
Fast, accurate claims payment is one of the ways we make a difference in people's lives. Claims professionals work directly with members, doctors and employer groups, providing a friendly and knowledgeable voice at the other end of the phone at times when it's most needed. Reviews and adjudicates complex, sensitive, and/or specialized claims in accordance with claim processing guidelines. Acts as a subject matter expert by providing training, coaching, or responding to complex issues. May handle customer service inquiries and problems. Reviews pre-specified claims or claims that exceed specialist adjudication authority or processing expertise. Applies medical necessity guidelines, determines coverage, completes eligibility verification, identifies discrepancies, and applies all cost containment measures to assist in the claim adjudication process. Handles phone and written inquiries related to requests for preapprovals/pre-authorizations, reconsiderations, or appeals. Ensures all compliance requirements are satisfied and that all payments are made against company practices and procedures. Identifies and reports possible claim overpayments, underpayments and any other irregularities. Performs claim re-work calculations. Makes outbound calls to obtain required information for first claim or reconsideration. Trained and equipped to support call center activity if required, including general member and/or provider inquiries.
Responsibilities
- Review and adjudicate complex, sensitive, and/or specialized claims.
- Act as a subject matter expert by providing training and coaching.
- Handle customer service inquiries and problems.
- Apply medical necessity guidelines and determine coverage.
- Complete eligibility verification and identify discrepancies.
- Assist in the claim adjudication process.
- Handle phone and written inquiries related to preapprovals/pre-authorizations.
- Ensure compliance requirements are satisfied.
- Identify and report possible claim overpayments and underpayments.
- Perform claim re-work calculations.
- Make outbound calls to obtain required information.
Requirements
- 1-2 years of experience in a production environment.
- Demonstrated ability to handle multiple assignments competently and accurately.
- Strong oral and written communication skills.
- Ability to maintain accuracy and production standards.
- Technical skills and analytical skills.
Nice-to-haves
- 2+ years of claim processing experience.
- Understanding of medical terminology.
- Strong knowledge of benefit plans, policies, and procedures.
Benefits
- Full range of medical, dental, and vision benefits.
- 401(k) retirement savings plan.
- Employee Stock Purchase Plan.
- Fully-paid term life insurance plan.
- Short-term and long-term disability benefits.
- Well-being programs.
- Education assistance.
- Free development courses.
- CVS store discount.
- Paid Time Off (PTO) and paid holidays.
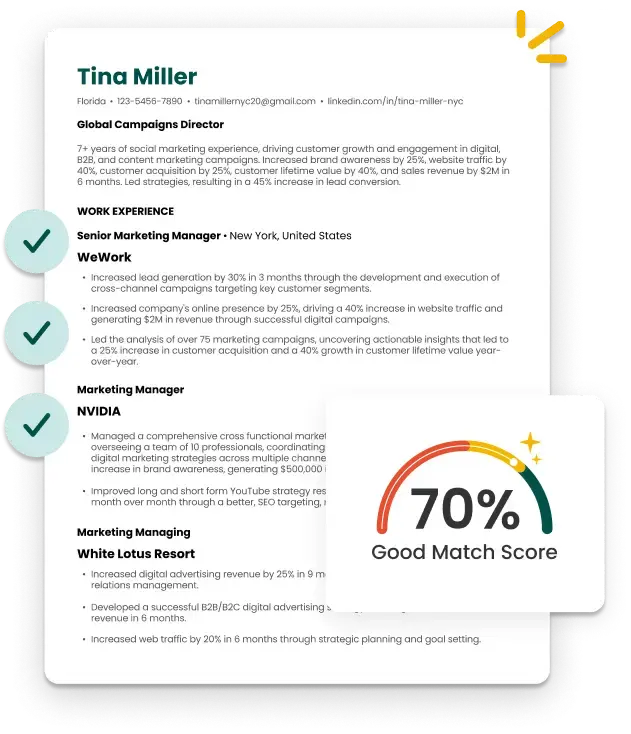
A Smarter and Faster Way to Build Your Resume